Why Dr. John Q. Cook Is the Right Breast Surgeon for You
Our patients benefit from Dr. Cook’s devotion to naturalism and extensive experience with breast surgery. He has performed thousands of operations with breast implants.
Dr. Cook is committed to an individualized analysis of each patient who comes to him for breast augmentation surgery. He considers your breast structure, your goals, and your activity pattern to find a solution that works for you.
We offer our patients a detailed analysis, which includes anatomical breast sizers and simulation software to help you visualize your potential results. We also have an extensive database of before and after photos that our patients have allowed us to share during the consultation process.
Dr. Cook’s experience with complex breast reconstruction surgery provides him with a wide range of technical refinements that he can use to optimize results for his breast augmentation patients.
Education and Credentials

Awards and Recognition

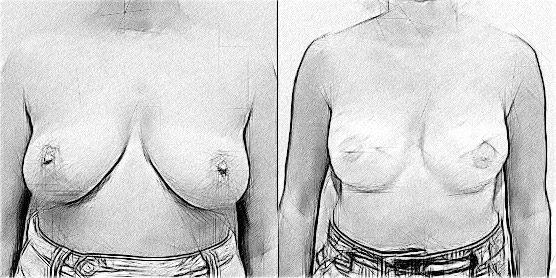
REAL PATIENT RESULTS
See the difference experience makes. View the full before & after photo gallery of Dr. Cook and his team.
Breast Reconstruction
Rebuild a Feminine Silhouette After Medical Treatments, Trauma, and More in Chicago and Winnetka
In his 30 years on the staff of Rush University Medical Center, plastic surgeon Dr. John Q. Cook has restored a pleasing form to hundreds of patients seeking breast reconstruction in Chicago and Winnetka. Patients at Dr. Cook’s Whole Beauty® Institute benefit from his extensive experience with breast reconstruction options, such as tissue expansion, breast implants, and the emerging technique of fat transfer. This experience allows him to help patients with congenital breast deformities such as Poland’s syndrome or congenital asymmetry as well as patients who have undergone mastectomy or lumpectomy.
Although Dr. Cook has extensive experience in immediate breast reconstruction surgery after mastectomy, he currently focusses on techniques of reconstruction with implants and fat transfer that can be carried out on an outpatient basis. He uses these techniques to help patients who have already undergone mastectomy and are now ready for reconstruction, as well as patients with congenital breast problems such as Poland’s syndrome and patients who are seeking revision of a previous reconstruction. For patients seeking immediate reconstruction, he can expedite referral to colleagues at Rush University Medical Center, one of the Midwest’s leading academic medical centers.
As a service to patients looking for information about breast reconstruction, Dr. Cook provides a comprehensive overview in this section of the website.
Contact Whole Beauty® Institute for more information about breast reconstruction in Chicago or Winnetka. Call 312-751-2112 or send a message online
Request a consultWhy Choose Dr. John Q. Cook for Breast Reconstruction?
Breast surgery represents one of the major areas of Dr. Cook’s interest and expertise—and all of his work in the field is built on the foundation of his extensive experience in the challenging area of breast reconstruction surgery.
“One challenge is the creation of a new breast after mastectomy or a congenital problem, but an equally challenging situation is where we must then take the remaining natural breast and shape it to balance the breast that we have created.” Dr. Cook explains.
His extensive breast reconstruction experience also benefits patients seeking elective surgery, including augmentation.
Why Undergo Breast Reconstruction?
Patients who come to Dr. Cook’s Winnetka or Chicago centers for breast reconstruction are typically seeking to restore balance and wholeness to their body image. Breast reconstruction surgery can powerfully affect a person’s sense of well-being, and the techniques can be applied to meet a wide range of patients’ needs. Some patients seek immediate reconstruction at the time of mastectomy. Others may have undergone mastectomy or lumpectomy in the past and are now ready to consider breast reconstruction.
Still other breast reconstruction patients experience significant abnormalities of breast shape and position that manifest themselves during the period of breast development. For example, patients with Poland’s Syndrome, which may run in families, tend to have one breast with a tight base that is significantly smaller than the opposite breast. Even during the teenage years, the opposite breast is unusually settled, similar to the breast of a woman who has nursed several infants.
In some breast reconstruction patients, the underlying pectoral muscle is underdeveloped. Another common abnormality of breast development is referred to as the tubular or tuberous breast. In this type of breast, the base of the gland is constricted, and the diminished breast tissue tends to protrude through an enlarged areola.
Another common reason patients choose breast reconstruction is congenital breast asymmetry. Patients with this problem have two normally shaped breasts, but a marked difference in cup sizes—for example, an A cup on one side and a C cup on the other.
What Goals Do Breast Reconstruction Patients Have?
Each breast reconstruction patient may choose to put these different goals in an order of priority that makes most sense to her, but it is important that all of the goals be considered. Dr. Cook came up with these eight breast reconstruction goals through a critical analysis of his own surgical results, as well conversations with his patients.
Since he has a referral practice, he also has the privilege of evaluating patients who previously underwent reconstruction by a variety of plastic surgeons who have different preferred methods of reconstruction.
Read More...
Breast Reconstruction Goal 1: A Breast that Has a Soft and Natural Look and Shape
When everything goes perfectly, breast reconstruction with autologous flaps— particularly those from the abdomen—comes closest to meeting this goal. There are, however, significant trade-offs (when compared to the other goals) that should not be dismissed lightly. Recent advances in implant-based breast reconstruction have significantly improved the quality of results, so that the best implant-based breast reconstructions now come very close to achieving the same natural results that can be obtained with abdominal flaps.
Breast Reconstruction Goal 2: A Breast That Is Balanced with The Body and with the Opposite Breast
It is often said that the best results with breast reconstruction some with bilateral breast reconstructions. It is much more likely that a surgeon will achieve a good degree of symmetry with a double breast reconstruction than when it is necessary to match an opposite natural breast.
The importance of this goal depends very much on your priorities. Patients with a reasonable degree of balance when wearing a bra or swimsuit are often happy with the result. For others, it is very important to achieve as much balance and symmetry as possible in the unclothed state.
If unclothed symmetry is important, it is usually necessary to balance the opposite breast with the reconstructed breast via an appropriate procedure, whether breast augmentation, breast reduction, a breast lift, or a combined augmentation and lift.
One important point is that even if the natural and reconstructed breasts are brought into good balance, they will tend to behave differently over time. Fastidious patients will often find it necessary to rebalance the breasts a number of years after the initial breast reconstruction surgery. This is particularly true for people who go through significant cycles of weight gain and loss.
Breast Reconstruction Goal 3: A Breast that Will Need to Undergo the Least Number of Revision Procedures
Dr. Cook believes autologous flap breast reconstructions has an edge when it comes to this goal, due to the inherent characteristics of breast implants. With all surgeries that involve implants, it is important to consider two important issues: breakage of the implant and capsular contracture.
All of the newer implants are filled with what is known as cohesive gel, which means the gel sticks together, even if the shell of the implant breaks. Still, it is desirable to replace a broken implant, which will require an additional surgery.
A condition called capsular contracture can develop in some patients who undergo breast reconstruction. This problem is characterized by the formation of an unusual amount of scar tissue around the implant. This tissue can tighten, making the implant firm and altering the breast shape. Breast revision surgery is necessary to fix this condition.
It is important to mention that not all autologous breast reconstructions go smoothly. Portions of the flap may not survive, and revision procedures will be necessary to remove the firm tissue that results, as well as to bring the breast into a better shape.
Breast Reconstruction Goal 4: A Breast with Natural-Appearing Skin and Limited Scar
For some breast reconstruction patients, their mastectomy will involve the removal of a significant amount of breast skin. With tissue expander breast reconstruction, it is possible to gradually stretch the remaining skin in order to compensate for the loss.
When it comes to flaps taken from the abdomen or back, an ellipse of skin is carried with the flap in order to replace the missing skin. The problem with this breast reconstruction approach is that the skin of the back and the skin of the abdomen have different coloring, thickness, and texture from the skin of the breast. This may produce a “patched” appearance that can be quite noticeable.
Some breast reconstruction patients may undergo more limited mastectomies, such as skin-sparing and nipple-sparing procedures, in which case the patched appearance can be avoided or minimized.
Breast Reconstruction Goal 5: Avoid a Difficult or Complex Recovery from Surgery
If this is the goal, both implant-based and expander-based breast reconstructions generally have an advantage over flap-based breast reconstructions, because the patient only has to recover in one area of her body.
With flap breast reconstructions, there is generally a significant recovery from surgery in the donor area, where the flap was taken. There may be local complications in the back and abdomen that require treatment and/or potentially delay chemotherapy, if that approach is needed.
It is sometimes possible to obtain an excellent breast reconstruction result with an abdominal flap, so that no further surgeries are necessary. Now, with skin-sparing mastectomies, this effect may be possible with implant-based breast reconstructions as well. As a practical matter, no matter which breast reconstruction method you choose, there is a high probability of additional surgery to refine the result and balance the two breasts.
Breast Reconstruction Goal 6: Do Not Affect Function of the Body in a Negative Way
The main negative effect of implant-based breast reconstructions in regard to bodily function takes place in the area of the reconstructed breast. There can be tightness around the implant, which affects range of motion of the shoulder. This may require physical therapy.
This is the goal where, in Dr. Cook’s opinion, flap-based breast reconstructions have the greatest probability of falling short and having significant long-term consequences. With the back flap (latisimus dorsi flap), the large muscle that sits below the scapula and hooks into the upper arm is released from its attachments near the spine and brought around to the mastectomy defect along with some overlying fat and skin. Some people consider this muscle expendable, but Dr. Cook does not agree. The latisimus muscle is very important in sports—for example, when pushing off with a ski pole and during many yoga poses. Proper function of this muscle is also important for people using crutches or a walker (e.g., some older people and those who have recently had certain types of surgery).
Abdominal flaps used in breast reconstruction can also be problematic. There are three main versions of this flap: With the TRAM flap breast reconstruction technique, one of the sit-up (rectus) muscles is detached at its bottom end, and the entire muscle is released except at the very top so that it can carry the fat and skin from the middle of the abdomen to the chest. There are vessels connected to the upper end of the muscle that provide a blood supply to the entire flap. With the FREE TRAM flap breast reconstruction technique, a smaller portion of the muscle is sacrificed, and the blood vessels that flow into the lower end of the rectus are detached and sewn to vessels near the breast. With the DIEP flap breast reconstruction technique, a smaller vessel that comes through the rectus muscle is used to provide circulation to the flap when it is sewn to the breast area.
In general, the DIEP flap breast reconstruction technique has fewer long-term effects on the strength of the abdominal muscles than the other abdominal flaps, but all of these breast reconstruction operations involve a disruption of the function of a very important section of the body. Everyone who has ever had back pain knows that the first line of therapy is to strengthen the sit-up muscles with physical therapy and exercise. If function of the rectus muscle is significantly affected, this will have long-term effects on body mechanics. The DIEP flap breast reconstruction technique has its proponents who claim that rectus function is preserved, but Dr. Cook seen too many examples to the contrary. These include people with abdominal bulges and significant weakness of the rectus muscle. One example is a yoga instructor who can no longer teach many of the poses that involve tightening the core muscles.
Breast Reconstruction Goal 7: Minimize Scar and Deformity in Areas other than the Breast
One of the key advantages of tissue-expander and implant-based breast reconstruction is that the only area involved by the surgery is the breasts. Flap-based breast reconstructions are essentially “robbing Peter to pay Paul.” At the very least, there will be scars in areas of the body other than the breasts, and these scars may be difficult to camouflage in swimsuits and certain cuts of dresses.
The abdominal flaps are sometimes described as having the advantage of a tummy tuck along with the breast surgery. This is true to a degree, but there are significant limitations. First of all, the scar sits at a much higher level than would be present with a true abdominoplasty. Second, abdominal flaps may weaken the abdominal support mechanism, unlike a true abdominoplasty, which is designed to improve abdominal wall support.
There are breast reconstruction surgeons who use flaps from the buttock or from the outer thigh to reconstruct breasts. There may be special circumstances where this makes sense, but there will generally be a significant negative effect on the area where the flap is taken from, both in contour and in scar.
Breast Reconstruction Goal 8: Avoid Big Complications
Dr. Cook often tells his breast reconstruction patients that there are big “C” complications and little “c” complications. Little “c” complications can be disheartening but are not a serious threat to health and well-being. Big “C” complications may involve time in intensive care and long hospitalizations.
In general, he has found that implant-based breast reconstructions tend to have little “c” complications, while flap-based breast reconstructions can occasionally produce more significant problems. Perhaps this is because flap-based breast reconstructions are long, complex operations that tend to involve more than one body area.
Important Breast Reconstruction Decisions to Consider
If you are considering breast reconstruction surgery, there are a number of important decisions you will need to make about your surgical plan. These decisions include the timing of reconstruction, the type of reconstruction, and the treatment of the opposite breast:
Breast Reconstruction Timing
If your surgeon has recommended mastectomy as the treatment for your breast cancer and you are interested in breast reconstruction surgery, the first decision you will need to make is whether to have immediate reconstruction or delayed reconstruction.
Immediate Breast Reconstruction After Mastectomy
The advantage of immediate breast reconstruction is that the main step of your reconstruction can be carried out as soon as your general surgeon finishes the mastectomy. The plastic surgeon will coordinate her schedule with your surgical oncologist at Rush. Dr. Cook can refer you to a team of oncologic breast surgeons and plastic surgeons at Rush with extensive experience in immediate reconstruction.
Different types of breast reconstructions can be done immediately after mastectomy. This includes reconstructions with implants and tissue expanders, as well as reconstructions that involve flaps from the abdomen or back.
When given the choice, many patients opt for immediate reconstruction. Even though the reconstruction is usually not complete with a single operation, it is a work in progress. This helps to give patients a psychological boost during the recovery.
Why Would A Patient Not Opt For Immediate Reconstruction?
Some patients feel overwhelmed by the number of decisions they need to make, and they may choose to just focus on treating the breast cancer and then deal with the breast reconstruction at a later date. Some patients have aspects of their breast cancer that will require aggressive treatment with radiation and chemotherapy, such that it may be better to carry out the breast reconstruction when they have completed this process. There are also patients who are perfectly comfortable with how their bodies will look after mastectomy and prefer to use a simple breast prosthesis that fits inside the bra.
Dr. Cook generally recommends that patients who have decided to undergo delayed breast reconstruction still come to see him for a consultation before the mastectomy. This is because the information he gives them provides a clear understanding of what the eventual reconstruction will involve, and this helps to provide peace of mind.
Delayed Breast Reconstruction after Mastectomy
Dr. Cook sees many patients for delayed breast reconstruction. A good number of them were either too overwhelmed at the time of mastectomy to consider reconstruction or had surgeries at hospitals where there was not a strong commitment to immediate reconstruction. Some had complex issues with their initial treatment that required such attention that it made sense to consider breast reconstruction at a later date.
Since he performs the vast majority of his breast reconstructions with tissue expanders and implants, the good news for his delayed reconstruction patients is that he can usually carry out all of the steps for delayed reconstruction as outpatient procedures with relatively quick recoveries.
There Are Two Very Different Possible Paths to Breast Reconstruction
Breast reconstruction can be achieved with two very different approaches. The method that plastic surgeons use most commonly is to place a tissue expander under the pectoral muscle and skin of the chest after mastectomy has been carried out. The tissue expander is an implant with a valve into which salt water can be added, gradually stretching the new breast to its desired shape and size. Then, the plastic surgeon replaces the tissue expander with a long-term implant and makes other adjustments to shape the breast in an outpatient surgery.
The other method of breast reconstruction involves the transfer of a patient’s own tissue, typically from the back or from the middle of the abdomen to the area of the breast. This is referred to as flap reconstruction or autologous reconstruction. It is necessary for the surgeon to maintain a blood supply to the tissue that forms the new breast. The two main ways of doing this are a) using a muscle that provides a lifeline to the flap via an artery and vein that run through the muscle and into the overlying fat and skin; and b) finding a set of vessels that nourish the tissue that forms the new breast and sewing these vessels to the arteries and veins near the breast.
Breast Reconstruction and Cancer
Although the elusive goal of a cure for breast cancer has not yet been achieved, we are fortunate to have a much wider array of options for breast cancer therapy than were available even five years ago.
Rush has long been a leader in the field of medical oncology, and we are grateful that our colleagues are able to provide therapies that in many cases can hold even advanced disease at bay. From a surgical perspective, many patients are able to take advantage of various techniques of breast conservation therapy, which may eliminate the need for mastectomy. There remains, however, a significant group of patients for whom mastectomy is still the best treatment option. For many of these patients, immediate breast reconstruction at the time of mastectomy (post-mastectomy breast construction) can lessen the stress of the treatment experience. For many patients who have undergone or who are about to undergo mastectomy, there is a sense of a double threat.
read more...
First, there is the potential threat to longevity that the breast cancer itself imposes—along with the associated concerns of family responsibility and the ability to accomplish life’s major goals.
Second, there is a threat to a woman’s sense of beauty, physical harmony, and sexuality. This second threat is sometimes neglected by the doctors who seek to cure the patient of her disease. The plastic surgeon can step into this void and help to complete her cure in the truest sense of the word through breast reconstruction surgery. A person is not “cured” until her sense of physical integrity and well-being is restored.
Several techniques are available for immediate breast reconstruction after mastectomy. These techniques can be divided into two general categories: those that make use of silicone gel or saline implants to provide volume for the reconstructed breast and those that require the movement of tissue from other parts of the body (so-called autologous techniques of reconstruction). If autologous tissue is part of the treatment plan, most plastic surgeons make use of either tissue from the abdomen or the back.
Potential advantages to the flap-based breast reconstruction technique include the natural fatty consistency of the flap and the avoidance of the possibility of implant-related complications. There is also the possibility of a single-stage breast reconstruction, as opposed to a breast reconstruction that requires several steps. As a practical matter, it is often necessary to go back and do “touch up” operations if one desires a good balance between the reconstructed and the natural breast.
Although some surgeons suggest an additional advantage to the abdominal flaps—that of providing a “tummy tuck”—this is not entirely so, due to the fact that the scar in most cases runs across the mid portion of the abdomen, since the key tissue for the flap surrounds the umbilicus. Also, in order to obtain the blood supply for the flap, some degree of abdominal wall compromise is often involved. In recent years, an increasing number of people have discovered the critical importance of balancing and strengthening the function of the core muscles through such techniques as yoga and Pilates. A patient contemplating the use of an abdominal flap for breast reconstruction should discuss the issue of core muscle function with her surgeon.
The other main technique of autologous breast reconstruction is the back flap (latisiums flap). With this method, a portion of the latisimus dorsi muscle (a very wide muscle from the upper and mid back) and often part of the overlying skin is moved from the back to the chest area to help reconstruct the breast. For most patients, a saline or silicone gel implant is placed beneath this flap in order to provide sufficient volume for the reconstructed breast. The skin that is carried with the muscle is used to replace the missing skin that was taken with the mastectomy. This flap can be useful in very thin patients where there is concern about providing sufficient protection of the implant in the lower pole of the breast.
In some breast reconstruction cases, just the muscle is taken, so that a second scar on the back is avoided. Even in this version of the flap, there are functional considerations. The latisimus muscle has important functions, particularly for athletes. The muscle plays an important role in certain motions, such as pushing off with a ski pole. There are also considerations of long term body balance when all or part of a functionally important muscle is sacrificed.
Tissue expander and implant reconstruction is well suited to the patient who desires immediate breast reconstruction after mastectomy, because the initial procedure—the placement of the tissue expander or implant—can be accomplished more quickly than either the back flap or the abdominal flap. Also, the recovery from the surgery tends to be easier, since the tissue expander method does not require the plastic surgeon to create scars in or remove tissue from other parts of the body.
For some patients, our oncologic breast surgeons at Rush can carry out skin-sparing and nipple-sparing mastectomies. This enables our plastic surgeons to provide direct-toimplant reconstruction at the time of mastectomy. In some patients, this involves placing the implant so that its upper portion is covered by the pectoral muscle and the lower portion is covered by acellular dermal matrix. It is also possible to place an implant in front of the pectoral muscle and cover it with acellular dermal matrix.
With tissue expander breast reconstruction, the plastic surgeon places a tissue expander beneath the pectoral muscle (the main muscle involved in push-ups) after the general surgeon has completed the mastectomy. Think of the tissue expander as a saline implant with a valve embedded in its surface. This allows the plastic surgeon to inject a small amount of saline solution into the expander at the end of the procedure. The valve will also allow the plastic surgeon to add additional amounts of salt water into the device, usually at weekly intervals. With this weekly addition of the saline solution to the device, the skin and underlying muscle will be stretched to create a breast of the appropriate size.
Tissue expansion is carried out in a series of office visits that start either two or three weeks after the surgery. Most breast reconstruction patients identify a particular day and time that is most convenient, and this becomes the regular expansion visit. Typical injections are about 60 ccs or 2 ounces of sterile salt water solution per visit. The goal is to move the expansion process forward at a good pace without causing unnecessary discomfort to the patient. If a patient needs either chemotherapy or radiation therapy after her mastectomy, the treatments usually begin several weeks after the initial surgery to allow sufficient time for healing. This tends to allow for between one and three expansions before the patient begins radiation or chemotherapy
Once radiation or chemotherapy is underway, most plastic surgeons hold off on further expansion until the therapy is completed. Chemotherapy rarely impacts the eventual result of tissue expansion in a negative way. The only disadvantage is that the expansion occurs over a longer time period, due to the pause during chemotherapy. Radiation therapy can be more problematic, because it can cause production of extra scar tissue in the treated area. This means that the skin is usually stiffer than in someone who has not received radiation.
In some breast reconstruction patients, this stiffer tissue may resist the forces of tissue expansion and make it difficult for the surgeon to create an ideal breast shape with the expansion process.
With tissue expansion, the patient is an active participant in the decision as to when the optimum volume has been reached. There will typically come a point where the patient feels that the breast has achieved its proper size. If both breasts are undergoing breast reconstruction, both expanders are brought to the same volume. If one breast is reconstructed, the patient has a number of choices regarding the management of the opposite breast when the second stage of the breast reconstruction is carried out. If the opposite breast is large and heavy, it may be best to carry out a reduction. If the opposite breast is lacking in volume, particularly in its upper portions, it may be helpful for us to place an implant behind the breast in order to optimize the balance between the two breasts.
For some patients with a settled opposite breast, a lift may be helpful. There are also many breast reconstruction patients who do not require any surgery of the opposite breast. Our goal is to provide each patient with a good background of information, so that she can select the proper combination of procedures for the second stage of breast reconstruction surgery.
In the case of an expander, once it is brought to its optimum volume, most plastic surgeons carry out several more expansions to create extra space for the implant. The breast reconstruction patient will then go through a resting period during which no further expansions are carried out. This period lasts from one to several months and allows the expanded tissue to relax.
During this period when the reconstructed breast is over-expanded, the patient can compensate by padding the brassiere on the side of the natural breast, so that balance will be maintained in clothing. The patient is now ready for the second stage of breast reconstruction. This stage is where the artistry occurs, since it determines the form of the reconstructed breast and also brings the opposite breast into balance—if that is desired by the breast reconstruction patient.
The second-stage breast reconstruction operation is carried out on an outpatient basis. A small portion of the mastectomy incision is opened, and the tissue expander is removed. A number of techniques are used to create the fold under the breast, so that a natural curve in the lower pole of the breast is obtained.
Plastic surgeons may also make use of fat transfer at this breast reconstruction stage in order to add structure to particular areas of the reconstructed breast. According to the patient’s preference, the surgeon will use either a silicone gel or a saline implant to provide the main volume of the reconstructed breast. It is at this second-stage outpatient procedure that the surgeon many also modify the form and structure of the opposite breast in order to obtain optimum balance, if this is the patient’s desire.
Many patients are pleasantly surprised by the relatively quick recovery after the second stage of breast reconstruction. Light activity is permitted after the first postoperative visit, which usually occurs three or four days after surgery. Patients who work can return to their job in approximately one week, as long as the work does not involve heavy physical activity.
At our Winnetka and Chicago centers, we encourage our outpatient breast reconstruction patients to return to gentle exercise, such as walking as soon as comfort permits. Soon after surgery, we instruct our patients in a series of exercises designed to keep the space around the implant from becoming too restricted. This is particularly important in patients who have undergone radiation. We long for the day when this wonderful surgery will no longer be necessary!
Immediate Breast Reconstruction Details
Immediate Breast Reconstruction with a Tissue Expander Followed by an Implant
This is a common sequence that plastic surgeons follow for breast reconstruction patients. At the first stage of reconstruction, the surgeon places a tissue expander partially covered by acellular dermal matrix as soon as the general surgeon completes the mastectomy. Several weeks after this surgery, the patient begins the process of expansion. You will visit your surgeon’s office, where saline solution will be added to the expander over a number of weeks, which stretches and shapes the new breast. The second operation is an outpatient surgery during which the plastic surgeon removes the expander, places a breast implant, and carries out fat transfer. If you are having a single breast reconstruction, you may choose to have surgery to balance the opposite breast to the reconstructed breast at this time. At a third operation, your surgeon will create the nipple and may provide additional fat to the breast.
If you come to see Dr. Cook to learn about breast reconstruction, but you have not yet selected a general surgeon, he will arrange for an expedited referral to one of the breast oncologic surgeons and the plastic surgery team at Rush. Everyone will make every effort to coordinate schedules so that the team can quickly proceed with surgery, if you desire.
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
read more...
You will be admitted to Rush University Medical Center the day of your surgery. The combined mastectomy and insertion of a tissue-expander for breast reconstruction will take several hours. Surgery will be longer if it is a double breast reconstruction.
During this first phase of your breast reconstruction surgery, your surgeon will inject long-acting local anesthetic to help block the pain reflexes. The goal is to minimize your discomfort during the recovery. After the operation, your surgeon will talk to you and your family to let you know that everything went well. Since you are waking up from surgery, your recollection of this conversation will probably be a little fuzzy.
You will most likely spend two nights in the hospital after this phase of breast reconstruction. Some patients are ready to go home the day after surgery, and some require an extra night’s stay.
The plastic surgery team will visit you in the morning on your first day after surgery. Your plastic surgeon will review with you things that you can do to optimize your recovery after this phase of breast reconstruction.
When you leave the hospital, you will be protected by a dressing that resembles a bulky tube top and is held in place by a gentle stretch bra. You will most likely have one or two drains, and you will know how to care for them. You will keep the dressing in place until your first postoperative visit to your surgeon’s office several days after discharge. His team will contact you at home to see how you are settling in, and they are always available for your questions.
Your team will see you several times in the first weeks after the initial breast reconstruction surgery. They will remove any drains and give you instructions for exercises to avoid tightness in the area under your arm. They will guide you to a smooth return to light activity, and they will let you know when it is safe to return to more vigorous exercise.
The actual tissue expansion portion of the breast reconstruction process begins around the third week after surgery. You will find a convenient day and time to come in for weekly expansions. During your expansion visits, your surgeon will follow your progress with healing, return to complete activity, and arm motion.
For some breast reconstruction patients, additional treatment, such as chemotherapy or radiation therapy, will be necessary. Once these treatments begin, you will take a break from tissue expansion and resume expansion once your therapy is completed. We will give you specific guidelines that are based on your precise treatment plan.
When you have completed the stretching process of tissue expansion, you will have a rest period and then proceed to the second stage of breast reconstruction. This is an outpatient surgery. During this phase of breast reconstruction surgery, your surgeon will remove the expander, place a breast implant, and possibly carry out fat transfer. This is also the time when he or she will modify your opposite breast, if you desire, in order to balance the reconstructed breast. This may consist of a reduction, a lift, an augmentation, or a lift with augmentation.
If Dr. Cook performs the second stage of your breast reconstruction, you will come to see us three or four days after the surgery. We remove the dressing and fit you with a gentle support bra. Most patients are able to return to light activity, including work if desired, within several days of this visit. Even though the recovery from this second breast reconstruction surgery is generally easier than expected, it is important that you be gentle with your body and maintain a mild level of activity. We will give you specific instructions based on the particular surgery that you undergo.
Nipple reconstruction is a powerful step in breast reconstruction. It is usually best to wait for the breasts to “settle in” so that the placement of the nipple or nipples will be optimal. Dr. Cook often adds additional fat to the reconstructed breast at the time of nipple reconstruction. He will occasionally make minor modifications in the reconstructed breast or the natural breast to optimize balance and shape.
Our breast reconstruction patients return very quickly to light activity after nipple reconstruction. It is important to protect the nipple during the healing phase with a simple “bumper cushion” dressing, which we will explain to you.
Once the nipple is healed, we will provide color to the reconstructed nipple and areola during a visit to the office. Patients almost always report being amazed by the power of this simple step.
Immediate Breast Reconstruction with a Flap From the Back or the Abdomen
The two main flaps plastic surgeons use for breast reconstruction are the abdominal flap (which takes fat and overlying skin, if necessary, from the central abdomen) and the back flap (which involves a large muscle from the back with an overlying ellipse of skin and fat).
Read more...
With the abdominal flap, the plastic surgeon takes excess skin and fat from the central abdomen and moves it to the breast. The blood supply to this flap comes from vessels that run along the length of the rectus (sit-up) muscle and travel up from the muscle to the overlying fat and skin.
There are several ways to keep a good blood supply to the flap. One option is to free up the entire rectus muscle from its fascia and keep the muscle attached at its upper end beneath the ribs, while releasing it at its lower end near the pelvis. The muscle and the attached fat and skin are passed through a tunnel into the area of the breast and trimmed to the appropriate dimension. The other option is to rely for circulation on the vessels that enter the lower end of the rectus muscle (free TRAM or DIEP flap). These vessels and a section of the muscle with overlying skin and fat are carefully released and the vessels are cut and attached to vessels near the breast with microsurgical techniques. The area from which the flap was taken must be carefully repaired.
With the back flap, the latissimus dorsi muscle (commonly referred to as the lat) is used to carry skin and some fat to the area of breast reconstruction. The muscle is released from its attachments near the spine so that it can be brought around to the chest. The blood supply comes from vessels that enter the muscle near its attachment at the base of the arm, and these are carefully protected. Some women carry enough fat in the back area to supply the necessary volume for the reconstructed breast. More commonly, an implant is placed beneath the flap.
As you can imagine, the recovery from breast reconstruction surgery with the abdominal flap and the back flap is considerably more involved than when tissue expanders and implants are used. At the very least, there will be several more days of hospitalization and a longer period before a patient can return to normal activity. There are also additional scars to contend with, either on the back or on the abdomen, as well as potential longterm functional issues that should not be ignored.
Delayed Breast Reconstruction Details
If you are ready for delayed reconstruction, you have already completed the important step of treating your breast cancer. This treatment may have involved some combination of chemotherapy, radiation, and surgery. Many of Dr. Cook’s patients who have undergone delayed breast reconstruction tell him that the surgery helps to allow them to put the cancer behind them and feel like they are truly a cancer survivor.
Delayed Breast Reconstruction with Tissue Expanders and Implants
For most patients who are referred to Dr. Cook for delayed breast reconstruction after mastectomy, it is possible to carry out the entire reconstructive sequence in a series of outpatient surgeries, with relatively quick recovery.
Read more...
Dr. Cook’s first step when he assesses a patient for delayed breast reconstruction is to evaluate the skin in the area of the mastectomy.
If there has not been radiation to the area and the skin and fat underneath are of good quality, he will typically recommend starting with a tissue expander. If the skin of the area seems thin or if there has been radiation, he will start with a preliminary fat transfer to the area, as this significantly improves the quality of the skin. He sometimes prepares the skin with an external stretching device, which improves the amount of fat he can transfer. If Dr. Cook feels that the skin quality is not suitable for expansion, he can refer you to one of his colleagues in the Division of Plastic Surgery at Rush University for autologous reconstruction.
When Dr. Cook places the tissue expander, he often will carry out a fat transfer to the area, whether or not there has been a previous fat transfer to prepare the area. The recovery from the surgery where he places the tissue expander is generally quite easy.
There are some surgeons who categorically reject tissue-expander and implant-based breast reconstructions if there has been radiation after a mastectomy, but Dr. Cook has found these procedures to be suitable in some patients.
Each patient must be assessed individually, since flap-based breast reconstructions often have significant negative consequences on body mechanics that should not be ignored.
Tissue expansion typically starts three weeks after placement of the expander. The patient usually comes in weekly until the breast has reached the proper size.
For some patients who are referred to Dr. Cook for delayed breast reconstruction, the original surgeon preserved enough of the original skin that it may be possible to provide a direct-to-implant reconstruction.
Delayed Breast Reconstruction with a Flap From the Back and the Abdomen
The remaining steps are the same as immediate breast reconstruction.
When flaps are used for delayed breast reconstruction, the surgeon will open the previous mastectomy incision and lift up the skin to create a space for the flap. The details of the flap operations are the same as immediate flap breast reconstruction.
When tissue expanders are used for delayed breast reconstruction, the procedure is an outpatient surgery with a relatively easy recovery. This is not the case with flap-based breast reconstruction. The patient will need to spend several days in the hospital, and it will take quite some time to return to comfort in the back and abdomen. There is also the possibility of long-term functional issues.
Shaping the Opposite Breast with One-Sided Breast Reconstruction
For many patients, it is important that the reconstructed breast and the natural breast have a similar size, position, and shape. In order to achieve this, Dr. Cook will select from a portfolio of breast reconstruction techniques and design an operation is suited to the individual’s specific needs. In two-stage breast reconstructions, he will usually shape the opposite breast in the second operation, during which he removes the tissue expander and places the long-term implant for the reconstructed breast. There are some surgeons who like shaping the opposite breast at the time of placement of the tissue expander.
Implants can help to balance the reconstructed breast with the opposite natural breast, particularly in the upper pole. Natural breasts tend to become somewhat hollow in their upper portions with the passage of time. Reconstructed breasts will have a greater degree of upper pole structure, with any type of breast implant. An implant on the side of the natural breast will help make the upper portions of the breasts more balanced and stable over time. If the natural breast has become deflated due to life events such as weight fluctuation or pregnancy, an implant will restore tone. This can work well as long as the structure of the breast is not too settled. Otherwise, a lift may be necessary in addition to the implant.
Read more...
Reduction to Bring a Large, Heavy Breast into Balance with the Reconstructed Breast
Reconstructed breasts tend to have a compact structure and are limited in terms of the realistic size that can be achieved, especially with implant-based breast reconstruction. If the opposite breast is heavy and settled, the imbalance between the two breasts will upset body mechanics and lead to significant back discomfort. Breast reduction will help to bring the two breasts into a better balance and is an important part of breast reconstruction surgery. The reduced breast will respond more to body weight fluctuations than the reconstructed breast, and it will settle to a lower position as time passes, so it may be necessary to perform additional surgery with the passage of time.
Different Lift Techniques Produce Different Breast Shapes
Periareolar mastopexy works well for pointed breasts that need just a little lift. This technique produces a more rounded breast, which is a better match for the fundamental shape of a reconstructed breast.
Classical lifts can work well in breasts that are very stretched out in their lower portions with a great excess of loose skin.
Structural lists provide an ability to restore volume to the upper portion of the breast without implants. While planning the second stage of breast reconstruction, Dr. Cook will analyze the structure of the natural breast and review the implications of different lift techniques on breast shape and balance.
Lift Combined with Augmentation Frequently Helps to Harmonize the Two Breasts
Very often, a breast reconstruction patient will benefit if Dr. Cook lifts the opposite breast and adds volume behind the entire breast structure. He places the implant in the plane under the pectoral muscle. A natural breast that is treated this way will have a structure that is closer to that of the reconstructed breast, and the two breasts will behave similarly as time passes.
Breast Reconstruction After Skin-Sparing Mastectomy
With skin-sparing mastectomy, the general surgeon carries out the mastectomy through an incision that runs around the border of the areola with a short extension. For some patients, this allows for a single-stage breast reconstruction. With a flap-based breast reconstruction, the breast is immediately filled with the transferred tissue. With implantbased breast reconstruction, the implant is placed so that the upper portion is covered by the pectoral muscle and the lower portion is covered by acellular dermal matrix. For some patients, it may be possible for the surgeon to cover the implant with acellular dermal matrix and place it in front of the pectoral muscle. For some patients, the opposite breast can be modified at the time of the immediate reconstruction. For others, it can be modified at the time of nipple reconstruction, which typically occurs several months later.
Single-stage breast reconstruction, although appealing, may not obtain the ideal breast shape for all patients, so it is often necessary to do additional “touch up” operations as time progresses. For this approach to be successful, there must be very close coordination between the general surgeon and the plastic surgeon. The ideal patient is a woman with relatively small breasts who will not require radiation to the area of breast reconstruction. For some patients, it may make the most sense to use a tissue expander at the time of skin-sparing mastectomy and to proceed with expansion and a later outpatient surgery with conversion to a long-term implant and fat transfer.
Breast Reconstruction After Nipple-Sparing Mastectomy
Immediate breast reconstruction after nipple-sparing mastectomy involves the placement of implants that are covered by the pec muscle in their upper portions and by acellular dermal matrix in their lower portions. It may also be possible to place the implant in front of the pec muscle. As with skin-sparing mastectomy, it is often desirable to carry out later fat transfer or other surgical adjustments in order to optimize the reconstructed breast.
The reconstruction of the nipple and areola, although a small step in terms of technical complexity, carries a very large degree of emotional and aesthetic power. When the nipple is restored, the breast truly becomes a breast. With this in mind, there is obvious appeal to the concept of preserving the natural nipple and areola. This is the basis of nipple-sparing mastectomy.
read more...
The concern with nipple preservation is that it might increase the risk that a woman might experience a new breast cancer, since some breast tissue remains. Remember that all of the breast ducts lead to the nipple and areola. There are some general surgeons and medical oncologists who categorically reject nipple-sparing mastectomy and others who are advocates in very specific groups of patients. No one suggests that nipple-sparing mastectomy is for every patient.
From the standpoint of the surgical oncologist, nipple-sparing mastectomy requires a change in surgical technique from that of the “standard” mastectomy. The usual incision across the center of the breast is avoided. One common approach is for the surgeon to make an incision along the fold under the breast and another incision under the arm. There is a natural plane of separation between breast structure and the fat underneath the skin, and the surgeon must preserve this fat in order for the skin to heal properly. The ducts that lead into the nipple must be carefully cored out, and many surgeons send a biopsy from the base of the nipple to make certain that they have not missed an area of breast cancer.
The ideal patient for nipple-sparing mastectomy is someone who has a relatively small breast, a small tumor that is not near the nipple, no family history of breast cancer, and who is not going to be treated with radiation. Some surgeons feel that nipple-sparing mastectomy is a reasonable choice for women who are considering prophylactic mastectomy.
Advances in Breast Reconstruction
Relatively recent developments in the field have improved the results of three areas in tissue-expander and breast-implant breast reconstruction: acellular dermal matrix, cohesive gel implants, and autologous fat transfer.
Acellular dermal matrix allows for an easier creation of a natural curvature to the lower portion of the breast, cohesive gel implants are less likely to create irregularities in the reconstructed breast, and fat transfer produces a soft, natural result.
read more...
Acellular Dermal Matrix In Breast Reconstruction
Acellular dermal matrix is a natural scaffolding derived from the inner, non-cellular portion of skin that has helped our patients in several important ways.
With immediate breast reconstruction, acellular dermal matrix allows the surgeon to place an implant or a tissue expander without restricting the curve of the lower pole of the breast. When Dr. Cook uses this material, he connects it to the bottom edge of the pectoral muscle and to the proper level of the breast fold.
Another important use of acellular dermal matrix is for the treatment of capsular contracture, the formation of a tight fibrous capsule that may occur around implants. For reasons that are not yet entirely clear, it is difficult for this fibrous tissue to form over the portion of an implant that is covered by acellular dermal matrix.
Autologous Fat Transfer In Breast Reconstruction
One of the significant challenges of implant and expander breast reconstruction is that there may be just a thin layer of skin over the pec muscle after a mastectomy has been completed. We have known for years that breast reconstructions would look much better if only we could somehow have more of a layer of fat to camouflage the implant. The results from a reconstruction might then be more like the results of an augmentation in a woman with very small breasts. Fat transfer opens up this possibility.
Dr. Cook has made use of fat transfer in his breast reconstructions for many years. He routinely places fat in the plane between the skin and muscle in the second stage of his tissue expander breast reconstructions, which is when he removes the expander and places the implant. This allows for a softer look that is more like the natural breast. Fat transfer can also be used to improve the overall shape of the reconstructed breast. Dr. Cook also uses fat transfer in patients who come to him for delayed breast reconstruction.
Dr. Cook may use fat to prepare the breast for complex delayed breast reconstructions, particularly if there has been radiation. The beneficial effect of fat on irradiated skin can be quite dramatic.
Cohesive Gel Implants in Breast Reconstruction
Cohesive gel implants are less likely to ripple or show irregularities in a reconstructed breast. They allow the surgeon to have better control of the projection of the reconstructed breast.
If you would like to have a consultation regarding breast reconstruction in the Chicago, Hinsdale, and Winnetka areas, or if you have questions for our team, please call 312-751-2112 or contact us online.
Request a consult
Three Significant Advances In Breast Reconstruction
In the last decade the most common method of breast reconstruction has been the placement of a tissue expander at the time of mastectomy. This is known as immediate reconstruction. After the general surgeon completes the mastectomy, the plastic surgeon places a tissue expander underneath the pectoral muscle and the fascia beyond the bottom edge of the muscle.
Breast Reconstruction with Fat Transfer
A Fat Transfer with Breast Reconstruction has been highly useful in enhancing the quality of results for our breast reconstruction patients. We have used the technique to help patients undergoing immediate reconstruction and delayed reconstruction and to rescue areas that have been damaged by radiation.
Dr. Cook's Practice Blog
Explore our practice blog to learn more about non-surgical treatments and plastic surgery procedures available at The Whole Beauty® Institute. Get tips and advice, and discover new ways to improve your health and beauty.
Dr. Cook's HealthGems Blog
Dr. John Q. Cook shares his personal thoughts on well-being, quality of life, and more in HealthGems—from his decades of experience in the industry, studying and working with advanced technology and techniques.
Whole Beauty Skincare
SkinShopMD.com was created by Board-Certified plastic surgeon, Dr. John Q. Cook, as a trusted source for high quality, medical-grade skincare products to protect and rejuvenate your skin.

Educational Information
Get informed about cosmetic plastic surgery procedures and rejuvenating non-surgical treatments to help you make informed decisions about your desired treatment based on your aesthetic goals.
Testimonial and Practice Videos
Schedule a Consultation
Schedule a consultation with board-certified plastic surgeon, John Q. Cook, M.D., to learn more about plastic surgery solutions that may be right for you based on your aesthetic goals.
"*" indicates required fields
Our Office Locations
Our locations in the Gold Coast of Chicago and Winnetka in the North Shore reflect our commitment to convenient and discrete concierge-level service.
Chicago Office
737 North Michigan Ave., Suite 760 Chicago IL 60611 (312) 751-2112 Entrance at 151 E. Chicago Avenue
Winnetka Office
118 Green Bay Road Winnetka IL 60093 (847) 446-7562
Located directly across from Indian Hill Metra Station